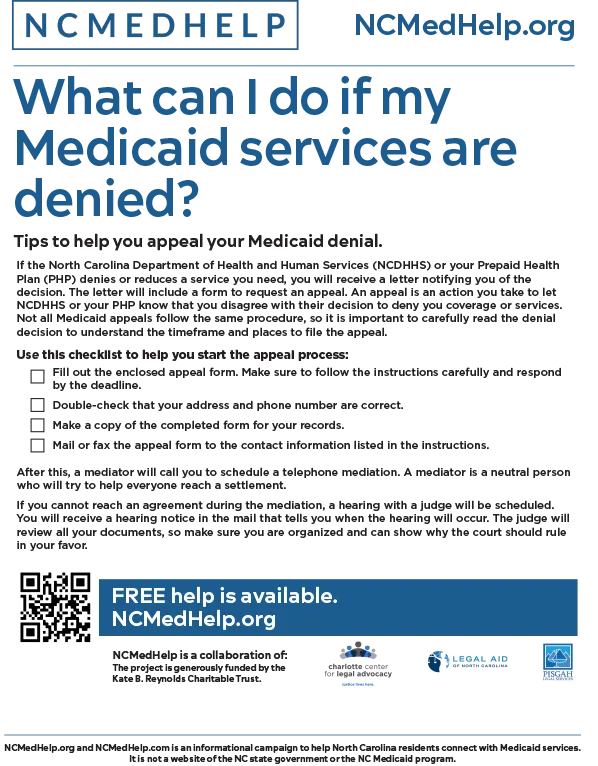
What can I do if my Medicaid services are denied?
Tips to help you appeal your Medicaid denial
If the North Carolina Department of Health and Human Services (NCDHHS) or your Prepaid Health Plan (PHP) denies or reduces a service you need, you will receive a letter notifying you of the decision. The letter will include a form to request an appeal. An appeal is an action you take to let NCDHHS or your PHP know that you disagree with their decision to deny you coverage or services. Not all Medicaid appeals follow the same procedure, so it is important to carefully read the denial decision to understand the timeframe and places to file the appeal.
Use this checklist to help you start the appeal process:
- Fill out the enclosed appeal form. Make sure to follow the instructions carefully and respond by the deadline.
- Double-check that your address and phone number are correct.
- Make a copy of the completed form for your records.
- Mail or fax the appeal form to the contact information listed in the instructions.
After this, a mediator will call you to schedule a telephone mediation. A mediator is a neutral person who will try to help everyone reach a settlement.
Do you have questions about how to use your Medicaid benefits or are you having trouble accessing care?
Contact our expert Health Benefits Resolution Specialists at 855-972-4357 (HELP) for free assistance today!
If you cannot reach an agreement during the mediation, a hearing with a judge will be scheduled. You will receive a hearing notice in the mail that tells you when the hearing will occur. The judge will review all your documents, so make sure you are organized and can show why the court should rule in your favor.
Free help is available across North Carolina. Request legal assistance and learn about your rights under NC Medicaid by contacting us today :